Is It Time to Rethink the Recovery Position in First Aid Training?
The recovery position is a fundamental part of first aid education. It’s a staple in training rooms, classrooms, and workplace courses, taught with confidence and often remembered with clarity. But at NR Medical Training, where every trainer is also a frontline clinician, we believe it’s time to ask an important question: has the recovery position become misunderstood, overused, and potentially misapplied?
In this article, we want to explore the real clinical purpose of the recovery position, the stories that highlight its misuse, and why a shift in both training emphasis and terminology may be overdue.
The Clinical Purpose of the Recovery Position
Let’s be clear about what the recovery position is for. It is an airway manoeuvre, intended for patients who are unconscious and breathing normally, when you need to leave them to get help or manage another danger. It positions the patient on their side, allowing gravity to assist in maintaining a clear airway, reducing the risk of obstruction by the tongue or aspiration of vomit.
That’s it. It is not a curative act, nor is it a default position for all unwell patients.
But too often, it’s applied with a level of enthusiasm that overlooks clinical judgement. The reality is that patients who are semi-conscious, confused, or even fully awake are being rolled into the recovery position when it simply isn’t appropriate. Worse still, the act of placing someone in the position is sometimes seen as the final step – a box ticked – rather than the beginning of a continuing assessment.
When Good Intentions Go Wrong: Clinical Stories from the Frontline
Every clinician at NR Medical Training has a story about the recovery position being misused.
I personally recall a tragic incident in a care home. Staff, freshly trained in first aid, proudly informed me that they had placed a resident in the perfect recovery position while waiting for an ambulance. On arrival, my crewmate and I found a beautifully positioned patient – but sadly, they had died. The technique had been executed correctly, but the patient had been left unattended and no one had recognised that they were no longer breathing.
This wasn’t incompetence. It was a result of well-intentioned staff relying on a rigid, oversimplified application of a technique without the clinical judgement to reassess or adapt.
Neil, NR’s co-founder, has countless similar stories. Conscious patients – even ones trying to sit up and talk – being rolled into the recovery position, because responders had been told it was the “safe” thing to do.
These aren’t isolated incidents. They’re indicative of a systemic issue in how first aid is taught.
Is the Name Part of the Problem?
We believe part of the issue lies in the name itself: "the recovery position".
Language shapes perception. Calling this posture the "recovery position" subtly implies that it’s a position that promotes recovery – that it stabilises, improves, or even treats the patient. It may foster an unconscious bias: that once someone is placed into this position, they are on the road to improvement and no longer require close monitoring.
That assumption is not just wrong – it’s dangerous.
The recovery position does not help someone recover. It is a temporary, passive airway protection technique. It does nothing to treat the underlying cause of the unconsciousness. It is not a final step. It is, at best, a stop-gap.
Perhaps we need a new name. "Lateral airway position" or "unconscious lateral position" may not sound as polished, but they better describe the function: maintaining airway patency in an unconscious person.
Supine Monitoring: The Case for Keeping Patients on Their Back
In clinical practice, unless a patient is at immediate risk of aspiration or airway obstruction, the supine position (on their back) is preferable.
Why? Because it allows for:
Direct visual and physical access to the airway
Continuous monitoring of breathing patterns
Easier access for airway manoeuvres, suction, or resuscitation
Immediate reassessment of responsiveness
A supine patient can be rolled if necessary – for example, if they begin to vomit. But keeping them on their back allows for much better clinical oversight and responsiveness. It also aligns with how we manage patients in emergency care settings: the vast majority are assessed, monitored, and managed in the supine position.
Teaching first aiders to keep patients supine whenever they can remain with them reinforces the importance of active monitoring and intervention – not passive positioning.
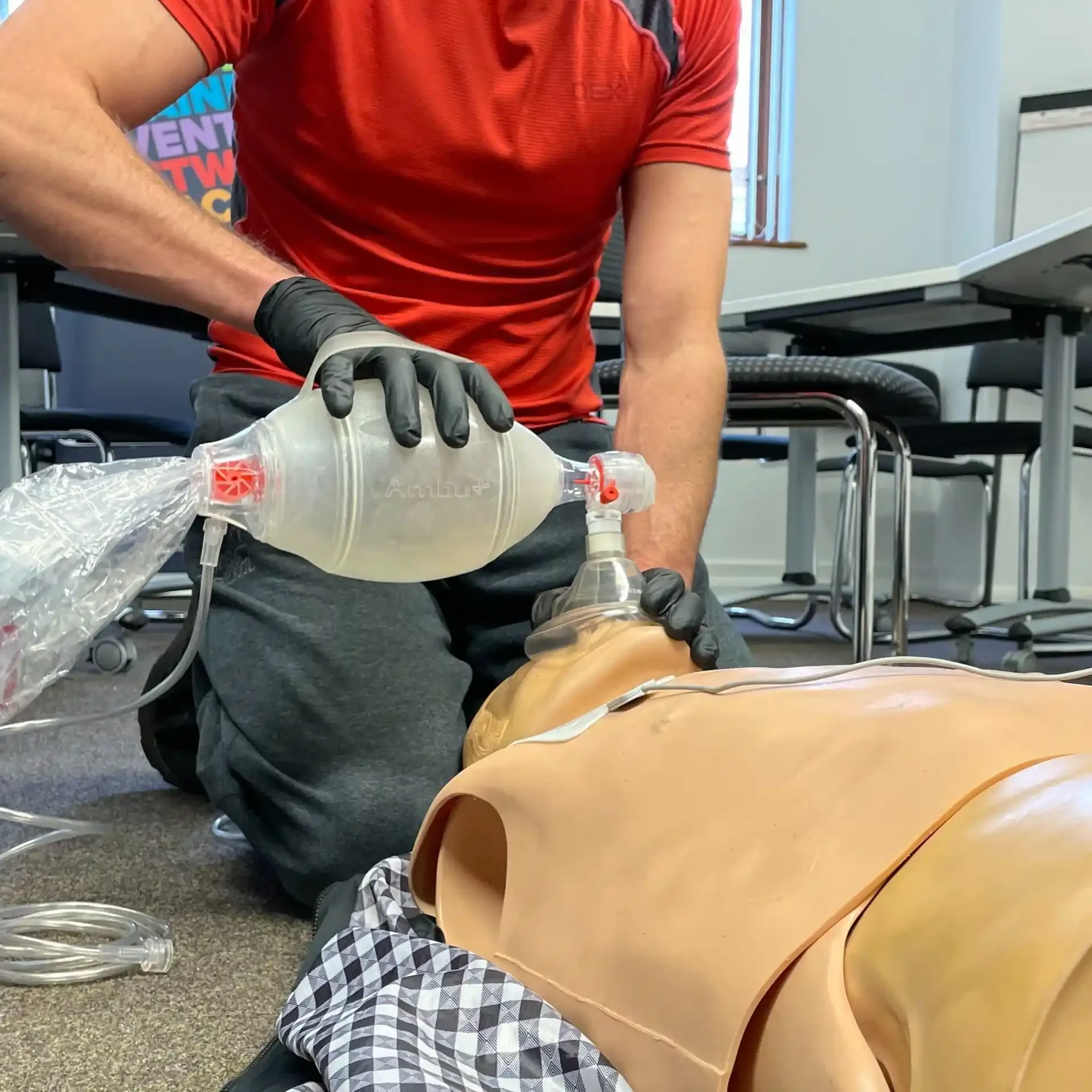
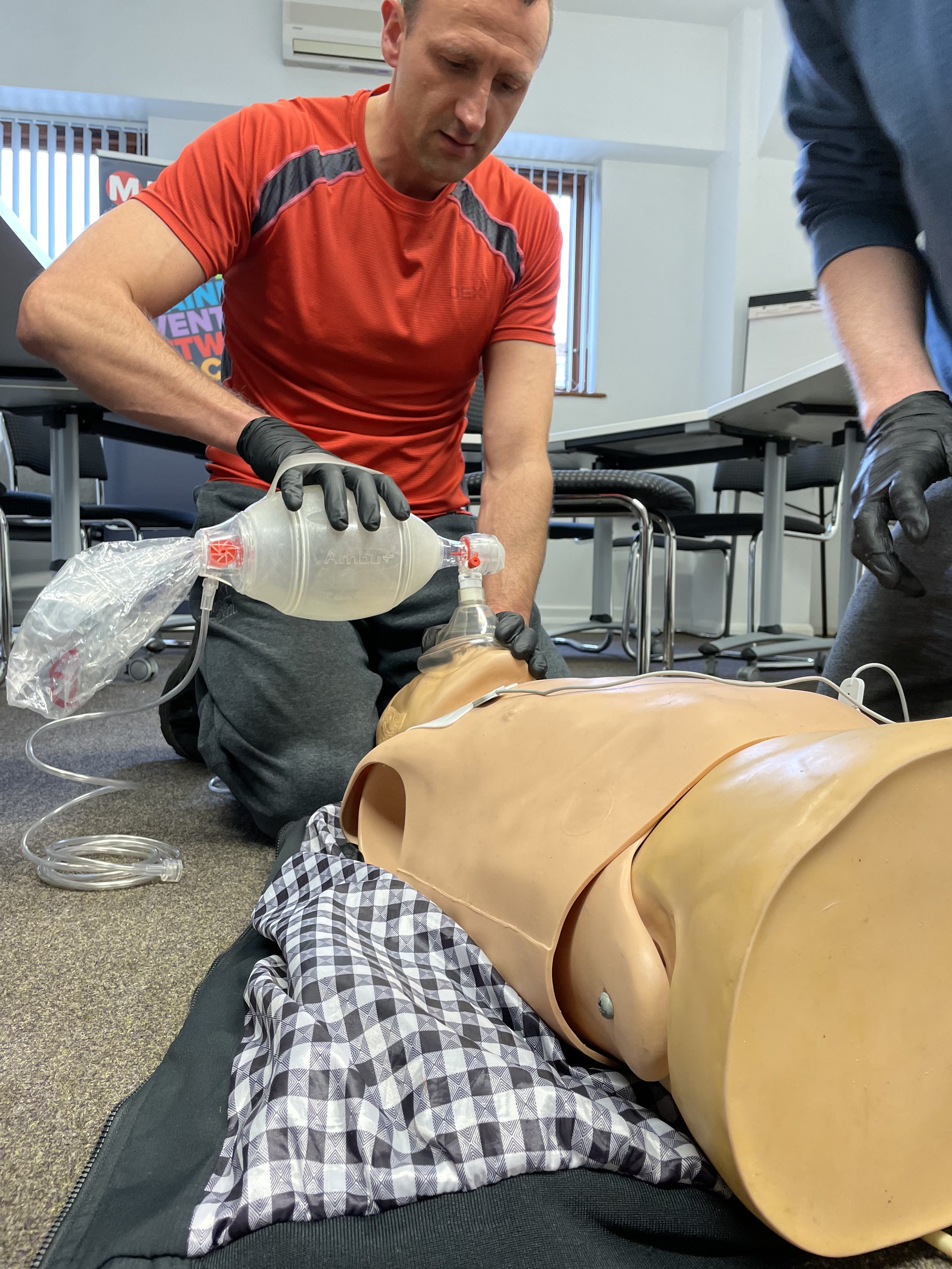
Postural Drainage: A More Useful Technique?
Postural drainage is a clinical term for using gravity to help clear the airway. This can be as simple as turning the patient’s head to the side, sitting them upright, or positioning the body in a way that allows fluids to drain without compromising the airway.
This technique is dynamic. It requires the responder to observe, adapt, and respond to changes in the patient’s condition. It reinforces that airway management is an active process.
By integrating postural drainage concepts into first aid training, we shift the focus away from rigid sequences and towards responsive, contextual care. It encourages first aiders to remain engaged with the patient and to treat the cause of the issue, not just perform a procedure.
Rigid Training vs Clinical Thinking
What we’re really talking about here is the difference between rote learning and clinical thinking.
The recovery position has been taught as a universal solution, a kind of medical reflex. But first aid isn’t a checklist – it’s a dynamic environment that requires continuous reassessment and judgement. That’s especially true in high-risk environments, such as care homes, industrial settings, or public spaces.
We believe training should empower learners to ask:
Is this patient unconscious and breathing normally?
Do I need to leave them?
Can I maintain their airway better in another position?
Am I able to monitor and intervene if they deteriorate?
If the answer to these questions doesn’t justify the recovery position, then it shouldn’t be used.
Recommendations for First Aid Training
At NR Medical Training, we’re not suggesting we scrap the recovery position. We’re suggesting we teach it differently:
Reframe it as an airway technique, not a default action.
Rename it, to reduce the unhelpful connotations of "recovery".
Teach the supine position as the preferred posture for responsive monitoring.
Incorporate postural drainage, head tilt, and responsive repositioning into basic airway management.
Train for judgement, not just memorisation.
Towards Smarter, Safer First Aid
The recovery position has its place. But it has come to symbolise more than it should. It has become, in some contexts, a ritual act – performed without sufficient thought, and with unintended consequences.
As clinicians, we have a duty to reflect on the real-world application of what we teach. And we must be willing to challenge long-held assumptions when they no longer serve patient safety.
It’s time to rethink the recovery position.